How To Pump Breast Milk for Your Baby: Babylist's Ultimate Guide
How often should I pump? How do I store breast milk? You have questions and we have ALL of the answers.

In This Article
Lots of breastfeeding parents also choose to pump breast milk for their babies. Whether you’ll be away from your little one for work or a trip, want to give someone else the chance to feed your baby or simply just need some time for yourself, there are lots of benefits to pumping. And for first-time and seasoned parents alike, there are also lots of questions.
From the best breast pumps and how often to pump to the logistics around storing expressed milk and how to make sure your little one will actually drink it, there’s no shortage of questions when you’re setting out to pump for your baby. This ultimate guide answers them all—and then some.
Why you might choose to use a breast pump
There are a few reasons why you may want to use a breast pump if you’re a breastfeeding parent:
You’re planning on being away from your baby either on a regular basis, such as for work, or for an extended period of time, like for a vacation or other trip.
You prefer feeding your baby expressed milk rather than breastfeeding.
You’re trying to maintain your supply of breast milk, either because your little one won’t or can’t nurse or you’re dealing with an illness or medication that isn’t safe for breastfeeding.
You’re struggling with low supply or engorgement.
How to choose a breast pump
There are many breast pumps to choose from, from hand pumps to hands-free electric pumps and everything in between, and figuring out what’s right for you can easily become overwhelming.
Types of breast pumps
There are four main categories of breast pumps:
Hospital-grade breast pumps. These are heavy-duty pumps that feature a powerful motor and a great amount of “sucks” per minute. They’re bulky and lack portability, but they do extract milk quickly and tend to be fairly quiet. Many breastfeeding parents choose to rent a hospital-grade pump instead of buy as they cost $1,000 or more.
Electric breast pumps. One of the most popular types of pumps, electric breast pumps require electricity to function (though some models run on rechargeable batteries and allow you to pump without being plugged in) and are efficient, portable and adjustable for both suction and speed. There are single and double models available, but most breastfeeding parents choose a double for efficiency.
Wearable electric breast pumps. Wearable pumps feature the newest in breast pump technology and have been gaining popularity over the last few years. Wearable pumps are completely hands-free; they slip right into your bra and let you pump while you’re busy doing other things. Each pump is made from a cup that fits over your breast, a flange and a milk collection bag all in one. They’re quiet and discrete but also expensive, and most pumpers find they don't express as much milk with a wearable than they do with a traditional pump.
Manual breast pumps. Manual pumps are affordable and portable. They work by the pressing motion of your own hand to create suction and pump your milk. Since there’s no motor, manual pumps are quiet and small but aren’t the best choice if you plan on pumping several times a day.
Most traditional breast pumps are made up of a few essential components: a flange that cups your breast and is often available in different sizes (these also are known as a breast shield); internal pieces like a valve and backflow protectors; a bottle or bag for milk collection; and a power source (a motor for electric pumps and a handle for manual models).
What type of breast pump is best?
There isn’t one type of breast pump that’s “best”; instead, it’s helpful to think about how to choose a breast pump based on what’s best for you and how you plan to use it.
Are you an exclusive pumper? You may want to consider renting an ultra-efficient hospital-grade pump to get the most out of your pumping sessions. Need to pump at work? A portable electric pump or a hands-free model may be a good choice for you. Don’t want to spend a lot of money since you’ll only be pumping occasionally? Look into a manual breast pump.
Here are a few factors to consider when you’re trying to choose the right breast pump for you:
Frequency. Think about how often you’ll be pumping. If you’re a working parent who will frequently be away from your baby or an exclusive pumper, you’ll be pumping quite a bit—so you’ll want a durable electric breast pump that can keep up. If you’re only planning on pumping once in a while, however, you’ll be able get by with a manual option.
Portability. Will you be commuting on public transportation with your pump and have to carry it along? Will you have access to an electrical outlet for your pumping sessions? Would you like the option to pump hands-free while getting other things done? Thinking these types of questions through before you choose your pump can be helpful as you make your decision.
Efficiency. A typical pumping session lasts about 10-15 minutes. If you’re crunched for time or know you’ll be pumping multiple times each day, a powerful, efficient pump can make a big difference.
Budget. How much do you want to spend on a breast pump? There’s a huge price range of pumps available—from about $20 to upwards of five hundred.
Features. Think through what features are important to you to help you decide on a pump. Do you want multiple suction settings? An option to switch out different sized breast shields? An ultra-quiet pump, or one that’s super easy to clean? One that’s compatible to the brand of bottles you’re using? A cord-free option? There’s a lot to think through, but it’s worthwhile to spend some time figuring out what’s important to you—and what isn’t—so you can make the right choice.
How do you get a free breast pump through insurance?
If you have insurance, the Affordable Care Act makes it possible to get a breast pump covered for free. Read about how to get a free breast pump through health insurance and visit Babylist Health to check to see if you're eligible. You may also be able to get free insurance-covered breast pump replacement parts through Babylist Health as well, so be sure to check!
When to start pumping breast milk
There’s no pressure to introduce pumping straightaway. “If baby and parent are together and breastfeeding is going well, there is no need to start pumping. Enjoy breastfeeding and snuggling with your baby. Rest whenever possible,” says Yines Garcia-Taylor BSN, RN, IBCLC founder of Prenatal Yini and a mom.
Garcia-Taylor recommends waiting at least two to three weeks after birth to introduce a breast pump. She also recommends starting slow.
“If a breastfeeding parent wishes to occasionally pump using a manual or an electric breast pump, they can pump right after breastfeeding for 10-15 minutes. This can be done once or twice a day. Milk output will be in small amounts, but remember, this is all bonus milk!” she says.
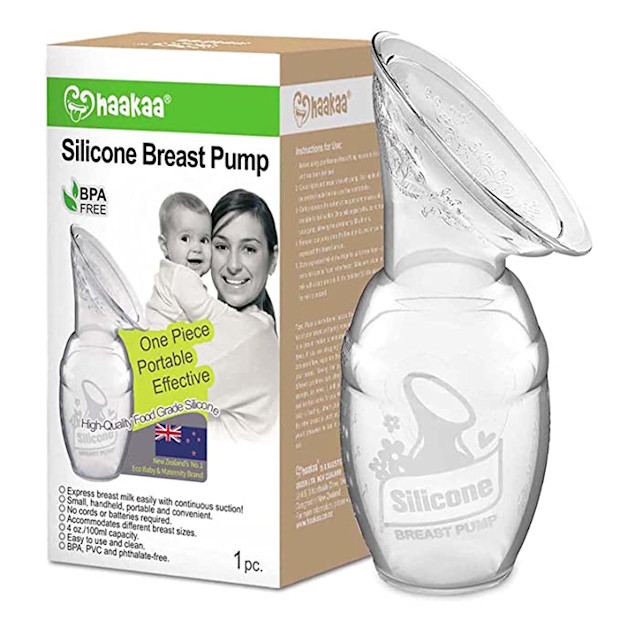
You can also begin by introducing a manual breast pump like the Haakaa. This type of pump attaches to your breast and uses suction to draw out the milk.
“It’s the easiest way to collect breast milk while baby breastfeeds on the opposite breast.”
One thing to keep in mind, according to Garcia-Taylor: be careful about pumping frequently after breastfeeding if you already have an adequate milk supply for your baby. It can put you at risk of developing an oversupply and, in turn, developing plugged ducts and mastitis (breast inflammation).
What if your baby goes to the NICU?
Pumping for a baby who’s in the NICU (the Neonatal Intensive Care Unit) looks a bit different than other types of pumping, according to Garcia-Taylor.
“If your baby is in the NICU, pumping within the first hour after birth (or as soon as the parent is feeling well) is important to start stimulating the breastfeeding hormones. Hand expression is best at collecting colostrum (the first milk after birth). I recommend NICU parents start pumping within an hour after birth if feeling well using a hospital-grade pump for 15 minutes followed by hand expressing for two to three minutes from each breast.”
Also, keep in mind that breast pumping helps with stimulating the breastfeeding hormones but is not efficient at removing colostrum.
How often to pump breast milk
For moms pumping and breastfeeding, Garcia-Taylor recommends pumping once or twice daily. One of these pumping sessions should be after the first morning breastfeed; that’s because prolactin levels (the hormone responsible for making breast milk) are the highest in the morning hours.
If you're feeding your baby only pumped milk, your exclusive pumping schedule should aim for about eight pumping sessions over a 24-hour period, including one overnight pumping session between about 2 a.m. and 5 a.m. And keep in mind that individual breast milk capacity differs and will affect how long and how often you’ll need to pump if you’re an exclusive pumper.
“Every mom has a different breast milk capacity. Parents with a larger breast milk capacity might have to pump less times daily to express the amount of milk baby needs in a 24-hour period, while parents with a smaller milk capacity may have to pump eight to 12 times daily to produce the same amount of milk. This is after milk supply has been established, usually six to 12 weeks postpartum. While establishing milk production, all breastfeeding parents should pump at least eight times each day, including one overnight session,” says Garcia-Taylor.
How long to pump breast milk
There’s no magic time limit for how long your pumping session should be, but on average, Garcia-Taylor recommends pumping for about 10-15 minutes per session if you’re a breastfeeding/pumping parent and 15-20 minutes each session if you’re an exclusive pumper.
You can also play around with your pump settings to figure out what works best for you. Some pumpers find that switching between expression and suction mode several times during a pumping session can initiate more letdowns, while others do fine with a static setting throughout. Don’t hesitate to experiment with settings and pump times as you find what works best for you.
How to clean pump parts
It’s important to follow specific guidelines for cleaning your breast pump. According to the CDC, wash your hands with soap and water for at least 20 seconds before you pump and be sure to inspect your breast pump to make sure there’s no dirt or mold in the tubing.
After each pumping session:
Fill a clean wash basin with soap and hot water and place pump parts inside—try to avoid placing your parts directly in the sink.
Scrub items according to your pump’s cleaning guidelines (most call for soap and water). Use a bottle brush that’s used exclusively for washing infant feeding items and nothing else.
Rinse your parts with clean water and allow them to air-dry thoroughly on a clean surface like an unused dish towel or clean paper towel. Don’t rub or pat them dry.
You can also clean your pump parts in the dishwasher and then allow them to air-dry as long as they are marked as dishwasher-safe. (You’ll want to use a heated drying cycle or a sanitizing setting if your dishwasher has one.)
How to feed a newborn pumped breast milk
Many parents choose to both breastfeed their babies and feed them expressed milk from a bottle. Understanding when and how to introduce a bottle of pumped milk to your baby can help make the transition from breast to bottle easier and more successful.
When is the best time to introduce a bottle?
Garcia-Taylor recommends following these tips when introducing a bottle to a breastfed baby:
Wait until breastfeeding is well-established—usually around three to four weeks after birth.
Use a bottle that’s designed especially for breastfeeding babies.
Use the paced bottle feeding method so baby won’t develop a feeding flow preference. (It’s easier and faster to get milk out of a bottle rather than a breast, so you’ll want to slow your pace when bottle feeding so your little one doesn’t overeat or develop a preference for the bottle over the breast.)
How to store breast milk after pumping
It’s important to be familiar with the guidelines for handling and storing breast milk properly, especially if you’re going to be feeding your little one expressed milk on a regular basis. This chart from the breastfeeding site KellyMom is an excellent resource on breast milk storage and handling. Bookmark it or even print it out and hang it on your refrigerator so you’ll have quick access to it whenever you need it.
Keep in mind these general tips when storing and handling breast milk for a full-term, healthy baby:
Freshly expressed milk is good for approximately four to eight hours at room temperature, but three to four hours is ideal.
Refrigerated milk, stored at the back, away from the door, is good for three to eight days, but about 72 hours is ideal. Thawed milk is good for 24 hours in the refrigerator.
Frozen breast milk should be stored at the back of the freezer, away from the sides and door, and should never be refrozen. Frozen milk is good for six months in a self-contained unit of a refrigerator and about 12 months in a separate deep freeze.
You can store your pumped breast milk in the refrigerator in either breast milk bottles or storage bags. If you’re freezing your milk, you’ll want to use storage bags and lie them flat to freeze—this will make them easier to store standing up after they’re frozen.
How to increase milk supply
One of the most common issues among breastfeeding and pumping parents is perceived low milk supply. According to Garcia-Taylor, it’s important to first determine if low milk supply is actually an issue before addressing it.
“Lots of pumping parents think they are not producing enough milk when in fact they are,” she says. “Milk output from pumping is not a true indicator of your milk supply. A breast pump is trying to imitate an efficient baby at the breast. Nothing compares to a well-latched baby,” she notes.
According to Garcia-Taylor, babies take about two to five ounces of milk per feeding from one to six months of age. This translates to one to one-and-a-half ounces per hour after your baby is one month old. For most pumping parents, expressing milk about eight times over 24 hours should be more than sufficient.
If you are experiencing low milk supply, Garcia-Taylor recommends reaching out for professional help from a lactation consultant. An IBCLC can work with you to use frequent pumping, massage and hand expression to increase your production.
Breast pumping tips
Pumping breast milk is hard work—it's helpful to learn all the tips and tricks you can!
Soothing sore nipples
Tender, sore and cracked nipples are a common struggle for pumping parents. Garcia-Taylor suggests these two fixes:
Use a comfortable suction setting on your pump. Many parents believe that when it comes to pumping, a higher suction equals more milk—but that’s not the case at all. Strong suction can cause nipple damage and doesn’t increase milk production. Use a comfortable setting that imitates your baby’s sucking on the breast (around 48-60 times per minute is generally recommended) and be sure to center your nipple inside the flange. You’ll also want to avoid your nipple elongating too much so it’s touching the end of the flange tunnel—this compresses your milk ducts and can make your pumping sessions less effective.
Use the correct flange size. A flange that’s too large or too small can be another common culprit of sore or cracked nipples. It can also lead to decreased milk collection. Garcia-Taylor recommends consulting a lactation consultant for a proper fitting. If you have insurance, check with your provider—many now cover up to six visits with an IBCLC.
Pumping at work
Pumping at work can feel stressful and overwhelming. Keeping these tips in mind can help make it a bit easier.
Choose the right pump. Consider things like portability, power source, noise level and privacy when you’re selecting a breast pump. Also think about how long you think you’ll be pumping.
Build a stash. Lots of pumping parents start pumping as soon as their milk supply is established (around four weeks or so for most people). This will allow you to stash away some milk and give you some peace of mind before returning to work. You’ll also want to introduce your baby to the bottle around this time and consistently offer it at least a few times each day so your little one gets used to drinking from it.
Know your rights. Get familiar with the Break Time for Nursing Mothers law so you know your rights as a pumping parent. Reach out to your supervisor or human resources department with any questions and to discuss the pumping accommodations at your particular employer.
Get prepared. A little prep can go a long way when you’re pumping at work. Think about what work-specific pumping products you’ll need; think through your pumping schedule; and figure out your options for storing your milk.
Invest in some accessories
You don’t need to stock up on a ton of products if you plan on pumping either exclusively or in tandem with breastfeeding—but there are a few key items that are worth investing in that will make your life as a pumping parent a lot more convenient.
Here’s what we recommend:
A good hands-free pumping bra does exactly what its name implies: it keeps your hands free (and your bottles in place) while you pump. You can also DIY this by cutting two small openings in the front of a sports bra.
Sturdy, double-zipper breast milk storage bags for your expressed milk.
A durable bottle brush to clean your pump’s nooks and crannies.
A cooler bag to keep your milk cool when you’re on the go or don’t have access to a fridge.
Other tips and tricks
Need some pumping encouragement along the way? These pro tips from our IBCLC can help you succeed as a pumping parent.
A positive mindset is vital. High levels of stress inhibit milk from flowing. Relaxation techniques, like deep breathing before and during a pumping session, can be helpful in relieving tension in the body.
Moist heat compress applied to breasts for about 10 minutes before pumping followed by gentle breast massage for 30-60 seconds encourages milk flow.
Always follow pumping with hand expression. Even if no milk comes out, don’t get discouraged, keep going. The more consistent you are the more milk you will see at each subsequent pumping session.
Breastfeeding is easier than pumping—but pumping is also breastfeeding!
For moisture inside the tubing, leave the tubing connected to the pump but not to the bottles and let the pump run for two minutes or until moisture clears out. If the tubing is moldy, replace it immediately.
And last but certainly not least, if you’re struggling with breastfeeding and/or pumping, please ask for help.