
Breast Milk Storage 101: How Long It Lasts + Where to Keep It
A quick, save-worthy guide to breast milk storage times for fridge, freezer, and beyond.

In This Article
There’s a lot to figure out when you’re pumping—like how long milk can stay out, how to freeze and thaw it, and what to do if your baby doesn’t finish a bottle.
As a certified lactation counselor (and a mom of two who’s been there myself) I know how overwhelming this can feel at first. I also spoke to Sandra Murray and Leah Tribus, both international board-certified lactation consultants (IBCLCs), to answer a few specific milk storage-related questions. This guide breaks it all down in a way that’s clear, supportive, and judgment-free.
Learning how to store breast milk helps keep it safe for your baby and preserves all the goodness you worked so hard to pump. And once you’ve got the basics down, it’ll start to feel like second nature.
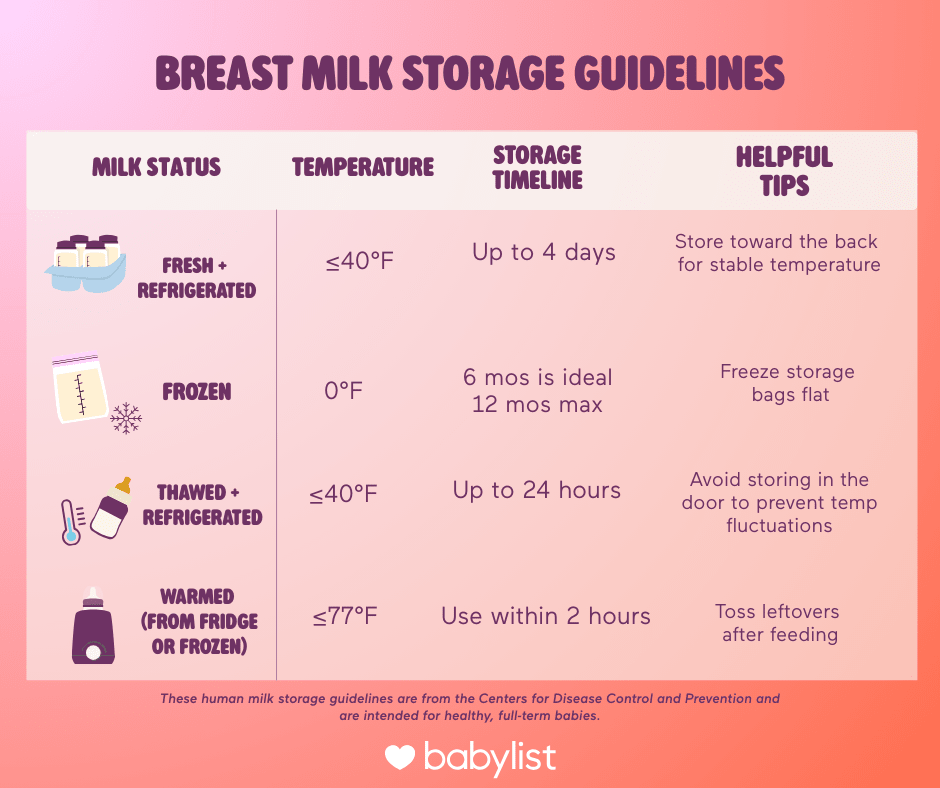
Breast Milk Storage Guidelines
You’re doing the hard part—pumping—here’s how to handle storage so none of it goes to waste. IBCLC Sandra Murray says breast milk is a living fluid, containing fats, enzymes, immune cells and beneficial bacteria. “Once pumped, these components change over time and at different rates when milk is left at room temperature, refrigerated, or frozen.” She adds that storage guidelines are based on what keeps breast milk both safe and at the optimal quality.
These guidelines from the Centers for Disease Control and Prevention (CDC) are a great place to start. They're meant for healthy, full-term babies, and they cover how long you can safely keep breast milk at room temperature, in the fridge or freezer.
Freshly expressed breast milk can be left out at room temperature for up to four hours, and if left out—versus stored in the fridge right away—is best for immediate use.
💡 CLC tip: If your baby is born preterm or has specific feeding needs, your healthcare provider might recommend more conservative storage limits—so don’t be afraid to ask what’s best for your baby’s situation.
Another rule that’s easy to remember? The “Rule of Fours” from the American Academy of Pediatrics (AAP):
⏱️4 hours at room temperature
⏱️4 days in the fridge
Just keep in mind that a few things—like how clean your pump parts are or if your fridge is really full—can impact how long milk stays safe. When in doubt, it’s best to err on the side of caution.
What to Store Breast Milk In
According to the CDC, the safest way to store pumped milk is in clean, food-grade containers with tight-fitting lids—think plastic or glass bottles, silicone or plastic milk storage bags, or trays made just for breast milk.
Below are the most common options, including some pros, cons and how they stack up for everyday use.
Breast Milk Storage Bags
These pre-sterilized, disposable bags are a popular pick for a reason. They're simple to use, easy to stash and make storing and freezing breast milk a lot more convenient—including those who want to create a freezer stash. Some allow you to pump directly into them, too.
Why it works:
Budget-friendly
Freeze flat to save space
Great for pumping at work or while traveling
What to consider:
Can leak if overfilled or not sealed well
Not reusable
Plastic or Glass Bottles
Another popular way to store milk is in reusable plastic or glass bottles. If your pump connects directly to bottles, you may even be able to pump straight into them—saving you time (and fewer dishes to wash later). Some options (like Medela and Gulicola, for example) can also be used as feeding bottles with their compatible collar and nipple.
Why it works:
Convenient (less transferring)
Leakproof and sturdy
Many are compatible with bottle warmers
What to consider:
Glass can break (though some come with sleeves)
Take up more freezer space
Slower to thaw when frozen
Breast Milk Storage Trays
These are like ice cube trays made for milk—each portion typically holds between half to one ounce depending on which brand you go with, and make it easy to pop a few out when you need it.
Why it works:
Less waste—you can thaw exactly what baby needs
Reusable
What to consider:
Takes up more space in the freezer
Cost adds up if you’re storing large amounts
More cleaning involved
Breast Milk Chillers
Milk chillers are insulated containers designed to keep pumped milk cold for hours when you don’t have access to a fridge or freezer. Depending on which one you choose, you either add ice cubes or use core that you refreeze after each use.
Why it works:
Perfect for pumping at work, traveling or running errands
Keeps milk cold for up to 20+ hours (depending on the brand)
Sleek, compact, and fits in most diaper bags
What to consider:
Pricier than a basic cooler bag
Usually only holds one or two bottles at a time
Ice cores need time to freeze before use
How To Store Breast Milk in The Fridge
Aside from the time guidelines mentioned above, there are also a few things to consider when storing breast milk in the refrigerator:
Where to place it. Store breast milk in the back of your fridge, where it’s the coldest. The temperature can fluctuate if you store them in the doors since they open frequently.
Always label the container or bag. It’s a good idea to get into the habit of labeling your milk with the date, volume and some parents like to note whether it’s AM or PM milk (which may have slightly different make-ups).
Use “old” milk first. When getting milk out of the fridge to feed your baby, you want to think first in, first out—so newer containers or milk storage bags should go to the back of the line.
How To Store Breast Milk in The Freezer
The CDC recommends using frozen breast milk within six months for best quality. That said, it’s still safe to use for up to 12 months if needed. Just aim for the older milk first and label everything with the date.
Once you’re in the groove, these tips can help keep things organized, make the most of your freezer space and cut down on waste:
Freeze in smaller amounts (2–4 ounces). That way you’re less likely to thaw more than your baby needs.
Leave room at the top. Breast milk expands when it freezes, so don’t fill bags or containers to the brim.
Freeze milk bags flat. They’ll stack better and save space once frozen.
Store milk in the back of the freezer. The temperature is most consistent there.
📌 Pro tip: If you’re exclusively pumping, a chest or deep freezer can give you more space (just keep in mind the storage timelines stay the same).
How To Store Breast Milk When You’re on the Go
If you’re pumping while out and about, you have a few options for keeping your milk cold until you get home. You can use a combination of breast milk storage bags or containers and a cooler or a breast milk chiller. And when you get home, transfer it to the fridge or freezer ASAP.
Practical Tips That Make Thing Easier
Keep these other tips in mind when storing breast milk:
No matter which container you use, always label your milk with the date, amount and baby’s name (especially if it’s headed to daycare). That way you can keep track of how long it’s been in your fridge or freezer and use the oldest milk first.
Once milk touches baby's mouth, you have a two-hour window in which you need to finish the bottle (due to bacteria from saliva).
Since breast milk naturally separates into a milk layer and a cream (aka fat) layer when stored, you’ll probably need to mix your milk before serving. Go ahead and swirl, mix or shake it—it won’t damage the milk at all.
How To Safely Thaw Breast Milk
You’ve figured out how to freeze your milk—now it’s time to talk thawing. The biggest thing to remember: use the oldest milk first. Frozen breast milk doesn’t go bad right away, but the quality can decline over time. Think “first in, first out” to keep things simple.
“Ideally, you could plan ahead for your needs across the next 24 hours,” says Murray. “You can just move the milk from the freezer to the refrigerator the evening before, [which] is a gentle way to thaw.” She says it also helps preserve some of the immune and nutritional benefits, which can be lost when you heat breast milk up past a certain temp (starting around 104 degrees).
There are a few safe ways to thaw frozen milk, according to the CDC:
Put it in the fridge overnight
Place it in a bowl of warm water
Hold it under lukewarm running water
You could also use a bottle warmer, just be sure to keep a close eye to make sure the milk doesn’t overheat.
🚫 Skip the microwave. It can create hot spots that could burn your baby’s mouth, and it may also break down important nutrients in your milk.
Once you’ve thawed your breast milk, here’s what to keep in mind:
Once breast milk is thawed, it’s best to use it within 24 hours—don’t worry if the timing gets tight; you’ve got some wiggle room if it stays in the fridge. The 24-hour countdown starts when there are no longer any ice crystals in the milk, not from the time you take the milk out of your freezer.
Once you’ve defrosted your milk, you’ll need to use it (aka you can’t refreeze it). The one exception to this is if your milk has started to thaw but still remains partially frozen. (Like in the case of a power outage, for example.) As long as there are still ice crystals present, it’s safe to refreeze your breast milk.
If you're ever unsure, a lactation consultant or your baby’s pediatrician can help you make the best call—there’s a lot of nuance here, and support can go a long way.
A note on high lipase breast milk
What if you’ve saved your milk, stored it properly and once you thaw and warm, your baby refuses it? For some people, thawed milk can look, smell or taste different from freshly pumped milk. Sometimes there’s no cause for this, but other times it’s because of something called excessive lipase activity, also referred to as high lipase.
Lipases are enzymes found in all milk that support a baby's ability to digest fats, protect against some infections and more. “During storage, especially in the freezer, these enzymes continue to act on milk fat, which can change the flavor over time,” says Leah Tribus, an IBCLC with The Lactation Network.
Milk with high lipase activity is completely safe for your baby to drink, but sometimes it smells and tastes soapy or fishy and a baby may reject it. Murphy and Tribus say you can try:
Mixing thawed milk with freshly expressed milk (“A 50/50 ratio often works well, and you can adjust based on your baby's preference,” says Tribus.)
Freeze your milk as soon as possible, to reduce the time the lipase as to do it’s thing
And they also note that everyone’s milk is different—some people might notice changes after a short period of time while others notice a change after several days. Murphy suggests taste-testing your freshly pumped milk every hour while refrigerated “to see when the flavor begins to shift. This helps you learn your personal ‘window’ for feeding and freezing.”
Pro tip: I ran into high lipase with my own stored milk and it really threw me for a loop. My top tip is to not wait until you have a freezer full of frozen milk to see if your baby will take it or not. Try thawing some frozen milk and giving it to your baby early on so you can head off any issues that may pop up.
The AAP recommends that parents may consider a scalding step if necessary, in order to save themselves from tossing milk solely based on taste. This essentially inactivates lipase activity
Here’s a quick how-to, but be sure to work with your lactation consultant if you feel like you need more direction.
Heat. Gently heat freshly expressed milk in a pot on the stove until small bubbles form around the edges, but don’t let it get to a full boil—aim for 180 degrees max
Cool. Transfer to a container to immediately cool in an ice bath (a stainless steel bottle works best here)
Store. Once the milk is cooled, transfer to your preferred storage container and put it in the freezer
Frequently Asked Questions
Have you done your research and you still feel a little overwhelmed? That’s totally normal. Figuring out how to properly store and thaw breast milk is nothing if not a little confusing. Here are some of the most frequently asked questions you may come up with—and their answers.
Frequently Asked Questions
My power went out! Now what?
If you’ve got a fridge or freezer full of breast milk, a power outage can feel like a nightmare. But good news: your milk might be okay longer than you think.
According to the CDC, milk stored in a full freezer is safe for about 48 hours. If your freezer’s about half full, it’s safe for around 24 hours. Milk in the fridge? You’ve got about four hours.
One thing to keep in mind: don’t open the door. Every time you peek, cold air escapes—and the temp drops faster. Keeping it shut helps preserve the cold.
If your milk is partially thawed but still has ice crystals, it’s safe to refreeze.
How do I store breast milk if I’m traveling?
Similar to if you’re storing pumped milk at work, it’s safe to keep your frozen breast milk in a cooler or other insulated container for up to 24 hours. Chilled breast milk that’s still within the 24-hour timeframe can then be either refrigerated or frozen.
If you plan to be away from your baby for an extended period of time, like a work trip or a vacation, check out Milk Stork. This breast milk shipping service offers domestic and international shipping for refrigerated or frozen milk. Some employers even cover the cost, so check with your human resources department beforehand.
Can I mix freshly pumped breast milk with milk that’s been in my refrigerator?
According to the CDC, you should not mix freshly pumped milk with already cooled or frozen milk. That’s because the warm milk can bring down the temperature of the stored milk. They recommend cooling fresh milk before combining it with any chilled milk that you’re storing.
Can I feed my baby expressed milk if I have thrush?
Thrush, a type of yeast infection, may grow on your nipple if you’re a nursing parent. It is safe to continue breastfeeding your baby and feed them expressed milk while being treated for thrush.It’s also safe to give your baby milk you froze while being treated for thrush. Some sources recommend not freezing pumped milk for later use during treatment while you have thrush for later use (because freezing milk does not kill yeast and there’s a risk of reinfection if you give the milk to your baby at a later date).
Expert Sources
Babylist uses high-quality subject matter experts to provide accurate and reliable information to our users. Sources for this story include:
Sandra Murray RN, MSN, BS-MCH, IBCLC, with The Lactation Network, a company that connects families with insurance-covered lactation consultations nationwide.
Leah Tribus, BSN, RN, IBCLC,with The Lactation Network, a company that connects families with insurance-covered lactation consultations nationwide.














